
People should be able to sign themselves off work for two weeks before asking a doctor for a sick note, doctors said.
At present, workers must give their employer a note from their doctor if they are off sick for more than seven days in a row, including weekends.
Writing so-called “fit notes” for people who only need to be off work for a couple of weeks takes away appointments from patients who may actually need them, Dr Richard Vautrey, deputy chairman of the British Medical Association’s (BMA) General Practitioners Committee.
On Wednesday, medics at the BMA annual meeting will vote on a motion calling for the “self-certification” period to be extended to 14 days.
This suggests people should be allowed two weeks off work without having to prove they have been ill.
Speaking ahead of the motion, Dr Vautrey said: “It’s about empowering patients and trusting patients and reducing unnecessary appointments with GPs.
“If you’ve got a patient who very clearly has an illness that is going to last 10 days to two weeks, why do they need to make an appointment with a GP just to get that note to tell their employer what their employer probably knows already and what the patient should be trusted to be able to pass on?
“This is just a motion that is trying to do something to reduce the unnecessary appointments that GPs have and thereby increase the number of appointments that are available for people who genuinely do need to see a GP.”
He said that if someone was to abuse the system it would be an issue between them and their employer, adding: “We just have to trust people to do the right thing.
“The vast majority of people want to work, they don’t want to be off work for significant amounts of time.
“If people are just needing those extra few days why waste a GP appointment when it’s not necessarily needed?”
Dr Vautrey said most patients with a self-limiting illnesses are usually better within a week but some need a bit longer to recuperate, for example if someone has sprained their ankle and does not feel ready to go back to work.
As well as fit notes for work, family doctors are also being asked to write notes for other “unnecessary” reasons.
Dr Vautrey said: “[One patient] could come in for a letter to say they are OK to take part in the school play or to appear on the stage in the local theatre. This is a fit 10-year-old child, why am I being asked to give them a letter?
“It’s like when patients are wanting to move house from one council flat to another because they have damp on the wall. That’s a discussion they should be having with their council housing team, they shouldn’t have to come for a GP letter. Actually, the council doesn’t think it is that worthwhile but they just fob patients off by saying ‘go and get a letter from your GP’ so it becomes this nonsense circular situation.
“Instead of going to the GP to get a letter to say ‘little Johnny shouldn’t be at school or he couldn’t attend his exam’, actually the parent should be able to provide those things.”
Commenting on the motion, Neil Carberry, director of employment and skills at the CBI, said: “When someone is sick enough to be off work for a week, they should try to see a doctor.
“The electronic fit note is a simple process to enable employers to understand how sick their employee is and what they can do when they return to work. Self-certification is only appropriate for short-term absences, when a doctor’s visit may not be required”.
READ MORE
Medics reject infection-reducing fist-bumps with patients to avoid ‘looking like rappers’
LGBT people face ‘significant barriers’ in end-of-life care, report finds
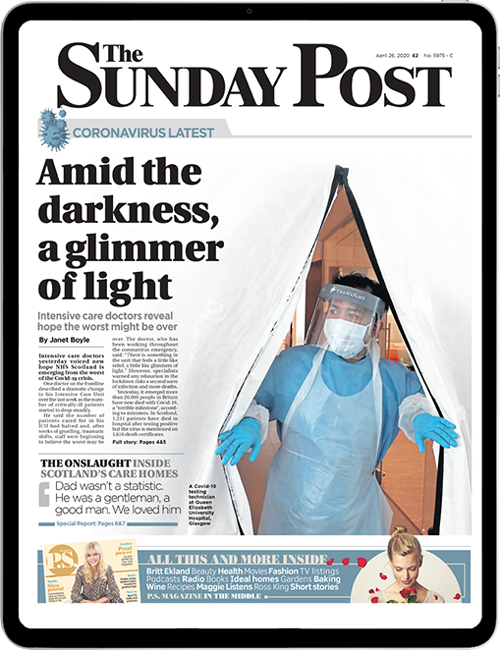
Enjoy the convenience of having The Sunday Post delivered as a digital ePaper straight to your smartphone, tablet or computer.
Subscribe for only £5.49 a month and enjoy all the benefits of the printed paper as a digital replica.
Subscribe