
One hundred and thirty one families have suffered devastating baby deaths and catastrophic injuries to infants and mothers at maternity units across Scotland in recent years, it can be revealed.
The new figures come two years after the Royal College of Midwives (RCM) warned the Scottish Government of the crisis in maternity services, prompting ministers to launch a taskforce.
Last December it emerged deaths of newborn babies in Scotland had reached a 15-year high.
Neonatal deaths
Scottish ministers ordered a review of neonatal death rates after two spikes over a six-month period in 2021/22. Completed in February, the review found no new or unusual causes of death, or systemic failures of care, were to blame, but said more comprehensive reviews of neonatal deaths were needed.
Midwives say this, and other recommendations, have yet to be implemented.
Meanwhile, a taskforce launched two years ago, chaired by Health Secretary Neil Grey and with senior nursing and midwifery representatives, continues to meet every three months.
Devastated mothers who have lost babies or suffered childbirth injuries say the response is “woefully inadequate” and there has been no information regarding progress made.
The new figures show 131 families have been paid more than £74 million by the NHS over the past five years.
The largest number of cases was with Scotland’s biggest health board, NHS Greater Glasgow and Clyde, which settled 62 claims for £25m. NHS Lanarkshire settled 18 cases for £18m; NHS Lothian paid out £6.1m and NHS Ayrshire and Arran £5.6m.
Conservative Social Justice Shadow Minister Miles Briggs has now called for an urgent parliamentary debate on the crisis. “Behind each one of these shocking figures is a real family who have suffered a tragic loss or injuries because of medical negligence,” he said.
“We know midwives and doctors have repeatedly raised concerns about resources and staffing levels. The fact so many families have received damages over the years appears to back up those views.
“While those figures represent money the hard-pressed NHS can ill afford, it’s the human tragedy behind every one of these cases that should give us most cause for concern. These damning statistics should go some way to jolting ministers into action.
“It’s been two years since the government launched a special taskforce to look at what is happening in maternity services, but we have heard not a whisper about what this taskforce has achieved.”
Mothers who have experienced loss and catastrophic injuries say it is shameful anyone should feel unsafe in a maternity unit.
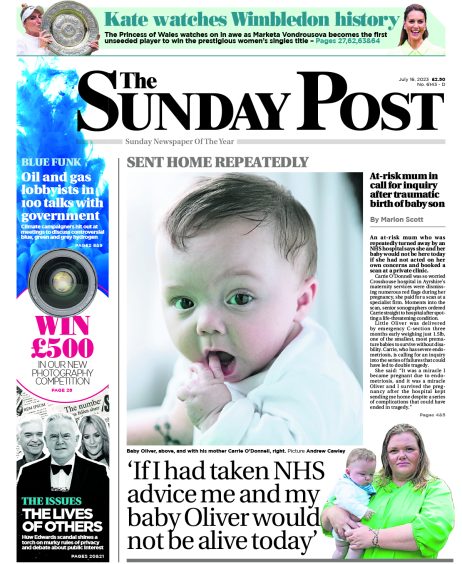
Two years ago, Carrie O’Donnell, 35, was repeatedly sent home from Crosshouse Hospital’s maternity unit in Ayrshire, when both she and her “miracle” baby Oliver could have died if she had not accessed a private scan that correctly identified a life-threatening condition.
In another case, hours after returning to Wishaw General’s maternity unit for the third time to be induced over Christmas 2022, doctors had to deliver the devastating news to Lynsey Hamilton that her baby daughter Carys had died inside her during the time she lay waiting in the hospital.
Lynsey, 34, had been showing all the signs of pre-eclampsia, a potentially dangerous condition that causes high blood pressure and protein in the urine.
Doctors then had to fight to save Lynsey, who is a Labour councillor on South Lanarkshire Council, as her blood pressure reached potentially fatal levels.
Lynsey said: “The very least mums and babies should expect is that our maternity units are safe, fully staffed and the equipment is the best that is available.
“Tragically, though, that is clearly not happening when there are shocking figures showing 131 cases have been settled throughout Scotland.”
Lynsey said that left her questioning how many “near misses” there had been. She said: “It is unacceptable for any maternity unit in Scotland to be short of staff. It is quite clear from the warnings midwives have already given the Government that investment is urgently needed.
“The Scottish Government do what they often do when faced with a problem – they launched a taskforce. This means it will likely take years before there is any substantial change when it is clear change is desperately needed now.”
Legal cases
Medical negligence lawyers say they are seeing an increasing number of high settlement cases involving baby deaths and injuries to both mother and child.
Michelle Adam, solicitor advocate and partner at major law firm Thorntons, said: “We are seeing cases where babies end up with catastrophic injuries that require large settlements because many of these children require lifelong care.
“One recent case involves foetal heart tracing equipment which was not reading a baby’s heartbeat. Maternity staff were unable to read the trace report, and that beautiful little boy was born with a hypoxic brain injury.
“He is unable to even sit in a chair by himself, and he’s growing into a big boy. He needs 24-hour care and will do for the rest of his life.”
The negligence expert said there were increasing numbers of Fatal Accident Inquiries involving baby deaths and injuries, and the number of medical negligence settlements remained high, with payouts having to take on board long-term care costs.
Adam said: “Sometimes cases are about a basic failure of equipment, which is something that really should not be happening in our maternity wards. I’ve seen cases where babies have suffered cuts during a C-section delivery. I’ve others where mothers have suffered injuries. One case recently involved a mother who wasn’t catheterised during labour and now her bladder is not working properly. This has had a dreadful impact on her life, including not being able to bond with her baby.
“Sometimes we hear about equipment not being monitored properly, or babies not being delivered quickly enough. The consequences can be devastating.”
Public Health Minister Jenni Minto said: “The Scottish Government is focused on improving perinatal and infant outcomes, including working with the established Scottish Patient Safety Programme perinatal and paediatric improvement programmes – one of the main aims of which is to reduce neonatal morbidity and mortality.
“Additionally, since October 2021, a National Hub has been in place jointly hosted by HIS (Health Improvement Scotland) and the Care Inspectorate. Its principal aim is to review and learn from the deaths of infants, children and young people in Scotland and to reduce future preventable child deaths.”
Labour’s women’s health champion Monica Lennon said: “There is deep concern over the lack of focus from the Scottish Government on maternity care. Midwives have repeatedly raised staffing issues and, unless this is tackled as a matter of urgency, there will be a negative impact on patient care. This is entirely the responsibility of ministers.
“The government has also failed to listen to everyone concerned about the downgrading of the multi-award-winning intensive care baby unit at Wishaw General, which will result in patients being sent miles away and cause mothers to be separated from their babies. It just does not make sense.”
Patrick McGuire, managing parter at Thompsons Solicitors which represents numerous cases involving young mothers and children said: “We agree with The Royal College of Midwives over their concerns over a lack of qualified and experienced staff and the impact that can have of Scotland’s maternity wards.
“This is one possible reason why we are seeing an increase in the amount of cases with disturbing outcomes. The Scottish Government must listen to midwives to ensure that our maternity wards are as safe as they can possible be.”
I can’t forgive mistakes or the way we’ve been treated
Carrie O’Donnell is just grateful she and her baby survived a potentially fatal childbirth condition after she was repeatedly sent home from hospital.
But both she and Oliver have suffered lasting injuries, and that is why she is one of the mums taking legal action against the NHS.
Carrie, 35, from Maybole, Ayrshire, was repeatedly discharged from Crosshouse Hospital maternity unit despite serious issues resulting from complications.
In November 2022 when she was told her baby had stopped growing, Carrie immediately sought a private scan as she felt Crosshouse had not given her an adequate explanation. Moments into the scan it was discovered that the baby’s placenta was breaking away, a potentially catastrophic situation which could have killed them both.
She said: “I was immediately rushed back to Crosshouse. Oliver was born at 27 weeks weighing just 685 grams. He was blue and so small he fitted into my hand. If it hadn’t been for that private scan, if I had gone home like the hospital ordered me to, we both could have died.”
Baby Oliver was one of the smallest and most premature babies in Scotland. She was not even allowed to touch him before he was whisked away from Crosshouse to a specialist high dependency baby unit at the Queen Elizabeth Hospital in Glasgow, where he remained for weeks.
Carrie says: “I cannot forgive the mistakes that were made and the way we have been treated since. As a result, I am now taking legal action against the hospital. I was very ill after the birth, but the level of treatment was appalling. I had to change my own catheter bags. Following the emergency delivery, I’ve been left suffering horrific pelvic pain which is affecting my mobility. I’ve had to seek private medical care because the waiting times and accessibility to specialists is so poor. Oliver is almost two years old now, but he is still in baby clothes for a six-month-old. His feet are turning inwards and we are having to get him specialist care and orthopaedic shoes.
“We are also waiting for appointments with a neurologist and an eye specialist to see whether long-term damage has been done. After all we endured, and all the mistakes that were made, last year hospital officials promised they would meet me to explain what had gone wrong. But I’ve heard nothing more.”
Midwives are struggling to give patients the best care
By Jaki Lambert, Scottish Director of the Royal College of Midwives
Our members are telling us that they are struggling to provide the best care they know they can deliver, the standard of care women deserve, because there simply aren’t enough of them or the time needed for them to develop the right skill mix.
For some time now, the RCM has raised concerns with the Scottish Government that maternity services are struggling. There was a government task force set up to tackle this as a direct result of last year’s pay negotiations. But we keep being told there will be no funding attached.
We are also concerned that recommendations to improve processes and reviews into serious adverse events which published prior to the neonatal deaths report in 2021/22 (which was published this year), have also yet to be implemented.
These included the introduction of resources for risk and improvement midwives so midwives can ensure that any learning from tragic events is identified and implemented at pace.
Crucially these midwives would also ensure the families who have lost their babies get the specialist support they need. We have met with the Cabinet Secretary and raised all these issues, specifically the delays in investigations and the impact that has on the families affected.
Understaffing undoubtedly compromises safety. The government has brought in laws to provide safe staffing and a methodology to identify the staff required.
However, when the directors of midwifery submit plans using this methodology, their plans are rejected.
This is having a direct impact on newly qualified midwives who are unable to find jobs.
The RCM’s student finance report has also laid bare the challenges our students face to become the midwives who will provide care for Scottish families for the next generation.
We have given the government solutions to the challenges highlighted in the RCM’s Five Year Forward Plan.
Our plan outlined the action required by the Scottish Government and NHS organisations in Scotland, as well as steps which need to be taken by the maternity profession to ensure our services deliver the highest standard of care to women and babies in Scotland. We urge the government to revisit our recommendations before it’s too late.
‘It is unforgivable that despite those tragic losses, nothing has changed for the better’
Rab Wilson is an award-winning public health campaigner whose whistleblowing led to a baby death inquiry at NHS Ayrshire and Arran seven years ago.
One of the most unforgivable aspects of the 2017 baby deaths inquiry is that health chiefs failed to learn lessons from the tragedies of the past.…but they did learn how to cover-up more effectively.
Scotland’s baby death numbers are the highest they have been in 15 years, and despite the dreadful six baby deaths that I helped uncover at NHS Ayrshire and Arran which led to a special inquiry, the fact that they have paid out £5.6million in negligence claims over the past five years shows very little has changed.
It is simply shameful that mothers and babies are still not as safe as they could be in our maternity units, and midwives are still having to raise concerns over the lack of staffing and investment after the damaging 2017 baby death inquiry.
The inquiry blamed the avoidable loss of six babies on staff shortages and a lack of specialist training, and here we are, in 2024, and babies are still dying and still being injured for exactly the same reasons.
My thoughts today continue to lie with the families who have lost loved ones through sheer negligence.
I got to know many of the families who lost babies at Crosshouse Hospital seven years ago, and I am very aware that those who suffer avoidable losses never recover from that trauma.
That is why it is unforgivable that despite those tragic losses, nothing has changed for the better.
Review investigators were highly critical of the lack of adverse incident reports made available to the public.
There were promises that this would improve right across Scotland and assurances that lessons would be learned to avoid the same mistakes being repeated.
Recent attempts by myself to access these reports found that instead of these being made readily available to the public, it is now even harder to find them never mind access them.
It appears that the only lessons learned from the tragedies of the past are lessons on how to hide the evidence from the public.
This is a betrayal of our NHS and all it stands for.
Those responsible for catastrophic errors much be held accountable, including high ranking health officials who have played a role in not ensuring adequate, safe staffing levels are maintained.
But we are less and less likely to see that happening in Scotland because of the way services are being run.
We have a government who thought it was acceptable to do away with the health watchdog we used to have and replace it with a system which has no teeth or power to hold anyone responsible.
Until we have a watchdog who can take proper action, we will continue to see babies dying, mothers being out at risk and mistakes being repeated.
Enjoy the convenience of having The Sunday Post delivered as a digital ePaper straight to your smartphone, tablet or computer.
Subscribe for only £5.49 a month and enjoy all the benefits of the printed paper as a digital replica.
Subscribe

 © Kate Darkins
© Kate Darkins