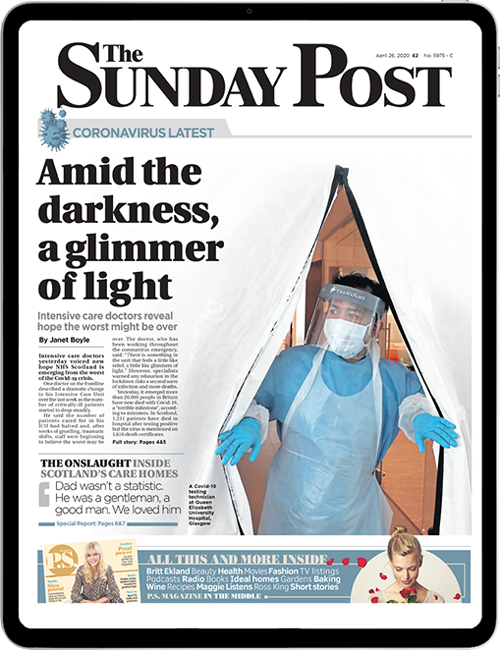
The long-lasting and life-changing legacy of Covid-19 is today laid bare as Scots victims describe how the virus has inflicted months of ill-health, exhaustion and mental anguish.
A series of interviews with Scots, some who have almost died after contracting coronavirus, detail the impact on their lives as experts call for urgent and systematic support for the thousands of patients facing a long, arduous recovery.
Most sufferers recover after about two weeks but around one in 10 people experiences prolonged illnesses. Some have remained ill for three or four months since catching Covid as a range of debilitating symptoms come and go.
Now doctors and patients are calling for more research into so-called “Long Covid” and want better help with rehabilitation from health services.
Many patients report having their concerns about ongoing health problems dismissed by their GP, while others have struggled to access appropriate rehab.
Researchers are trying to understand why some patients suffer from this slow, drawn-out illness while others fall seriously ill very quickly, suffering extreme breathing problems and need to be treated in a hospital intensive care unit. Some patients whose initial Covid-19 symptoms were relatively mild still suffer debilitating and lengthy after-effects.
Evidence of the sheer scale of Long Covid has come from the UK Covid Symptom Study, where people enter their ongoing symptoms in a smartphone app. The study is run by King’s College, London, and has 200,000 Scots signed up to report on their symptoms.
The app is run by professor Tim Spector, head of genetic epidemiology at the hospital, who said: “Many of these patients were not ill enough to be treated in hospital but are still experiencing post-Covid symptoms months after. Many improve after 90 days but one in 200 still have problems. That’s a lot of people affected.
“They are reporting double-vision, fatigue, shortness of breath and depression. We do not know why, but it could be that some people cannot get rid of the virus, that their immune system is not handling it well. Some people are still testing positive weeks later but are unable to pass on the virus to others. They are not infectious but their symptoms are persisting months later.”
Frontline medical staff report patients who were thought to have recovered from Covid-19 are turning up at hospital suffering from blood clots on their lungs.
Consultant Dr Dave Chung of Crosshouse Hospital in Kilmarnock, who is head of the Royal College for Emergency Medicine in Scotland, said: “I have treated at least two patients with blood clots in the lungs after they recovered from Covid. We know how to treat blood clots but those caused by Covid are new.
“The medical manual for treating the many post-Covid illnesses is being written as we go along. We now consider the impact of the virus when patients present as emergencies. Any serious breathlessness needs emergency treatment.”
Enduring breathlessness is a symptom reported by many Long Covid patients and professor Colin Berry of Glasgow University is leading a study on patients who are breathless and exercise-intolerant after C-19. The investigators will probe which patients are at risk of heart injury as a result of the virus and why only some patients suffer heart problems from the infection.
The study will also assess lungs and kidneys. Patients who have received any level of Covid hospital care will be studied.
Professor Berry said: “Some patients have been readmitted to hospital with chest pain, blood clots or other serious events after leaving hospital on recovering from Covid. Studies in Germany and London show changes in the hearts and lungs of patients who have had Covid.
“We also know that men have had more serious Covid infections and that women are more likely to be protected by oestrogen.”
Former GP and MSP Dr Richard Simpson is calling for research into the neurological effects of long Covid and a proper post-Covid assessments for people who have had the virus.
Dr Simpson, professor of health sciences and sport at Stirling University, said: “Careful follow-up is needed and a proper programme of post-Covid assessment vital. The consequences are not just neurological but cardiovascular and renal (kidney). We need to discover what part this might play in raising the risk of dementia and, if this is so, consider what other risk factors people have and limit those including obesity, smoking and alcohol.”
Scots are among the most obese in Europe, with 65% of adults overweight and 29% obese. “Research into those who have been on ICU ventilators shows that 30% will have some degree of psychological reaction and will need assistance to recover from this. We don’t have enough psychologists to treat those numbers of patients now needing this.”
Intensive care consultant Dr Ron Daniels, CEO of the Sepsis Trust, said a third of the calls it received were now for post-Covid illness: “The symptoms are similar to those experienced by people recovering from sepsis. One theory is that the body’s immune system goes into overdrive to fight off the virus, causing damage. Good research is vital to find the answers.”
Long Covid sufferer Barbara Melville told how she has struggled to get all the after-care she needs. Barbara, 37, first spoke to The Sunday Post about her enduring symptoms in May, 10 weeks after she was struck down by the virus.
She said: “I’ve managed to get some physio but still haven’t got a CT scan or lung function test. I’ve had some light physiotherapy support focused on pacing myself and gently building up to certain activities, like sitting up at my desk.
“Although I’m still not firing on all cylinders, it has drastically improved my quality of life.”
Dr Amy Small, a GP in Prestonpans, wants to see a multi-disciplinary team approach to treatment for patients. Dr Small, who fell ill with Covid-19 in April, is still ill five months later.
Writing in The Sunday Post today, she says: “We need to increase awareness and follow-up for patients. There are a whole host of people who were not hospitalised but are still struggling to recover the post-viral effects up to five months later.”
On Thursday, Health Secretary Jeane Freeman announced the setting up of a rehabilitation framework to help those recovering from Covid-19.
She said: “The rehabilitation and recovery of those who have had coronavirus as well as those who have been affected by lockdown is to be supported through a new rehabilitation framework.”
She added: “We know there is emerging evidence on the long-term effects of Covid-19 on people’s physical and mental health which is why it is vital that services supporting those who have been affected have rehabilitation and recovery plans in place.
“Our rehabilitation framework, which will be supported by the new National Advisory Board for Rehabilitation, will assist health boards, health and social care partnerships and independent and third sector organisations with this.
“It aims to build on good practice and capacity within the healthcare system and to explore innovative models, adopting a multi-disciplinary and multi-agency approach, to help ensure timely and flexible delivery of care and support to those who need it.”
Amy Small: We don’t know enough about it. We’re not doing enough about it
We need more research into the post-acute Covid-19 – or Long Covid – to allow us to better treat this disease.
Multi-disciplinary teams are needed to help patients experiencing a myriad of debilitating effects of the virus which linger for months after their first illness.
I speak from firsthand experience because both my husband and myself are Covid-19 “long-haulers” who have been struggling with the symptoms for five months since initially contacting coronavirus.
I first felt symptoms on April 11, the day after a colleague tested positive.
Testing was in its infancy and when I was eventually screened for it, I proved negative. I was tested immediately, almost too quickly. We now know that around 30% of tests give false negatives.
There is a theory that those who don’t have coughs are more likely to get false negatives, and I didn’t have a cough until day six. I did have headaches, a raised temperature, aching muscles and dizziness.
Since then, in total, I’ve worked half a day and was floored with exhaustion. My jaw aches after only eating cereal. My husband and I have gone from people who regularly ran up to 15K a week to being exhausted by a mile-long walk to our local nursery.
My experience shows just how much we still don’t know about the long-term after-effects of this virus.
We really need to increase awareness and follow-up for patients. There is a whole host of people who were not hospitalised but are still struggling to recover from the post-viral effects up to five months later.
Others, who were well enough to recover at home, have also gone on to suffer long-term effects of Covid-19.
We need multi-disciplinary teams to manage people with symptoms – ideally they would include neurologists, cardiologists, ear nose and throat surgeons, gastroenterologists, chest physicians, physiotherapists, occupational therapists and psychologists.
Indeed, all areas of healthcare which specialise in the post-viral effects, from gastro problems and breathing difficulties to hearing loss.
GPs, who are the first port of call for most long haulers, are really struggling to get on top of this.
We need treatment plans, much more information and more specialist help to allow patients to recover.
Amy Small is a GP in Prestonpans, East Lothian, and a member of the BMA’s Scottish General Practice Committee
Enjoy the convenience of having The Sunday Post delivered as a digital ePaper straight to your smartphone, tablet or computer.
Subscribe for only £5.49 a month and enjoy all the benefits of the printed paper as a digital replica.
Subscribe





 © enny Goodall/ANL/Shutterstock
© enny Goodall/ANL/Shutterstock