Scots suffering Long Covid fear a postcode lottery means effective diagnosis and treatment depends on where you live and on which side of the border.
An estimated 700,000 patients in the UK have described debilitating long-lasting symptoms after Covid, with many complaining the condition is little understood and treatment haphazard.
Scotland has not followed England in providing specialist centres for the debilitating symptoms, which can last for months after the virus – although some patients there complain finding effective treatment remains patchy – while health boards here promise to deliver treatment closer to home.
However, a survey of Scots health boards reveals a wide disparity in the treatment offered to patients as experts warn GPs struggle to know where to refer them.
Professor Kate O’Donnell, of Glasgow University’s department of Primary Care Research and Development, said: “It is difficult to get care and that is an issue. We are hearing this from GPs and it is difficult for them to know where to send patients. Finding a place to refer them is not easy.
“There is now a high awareness of Long Covid and a lot of discussion around the rehabilitation and research needed to treat patients. It is clear that many people have had damage to their organs. Many were fit and healthy before March last year.”
Professor O’Donnell and her team are launching research into Long Covid patients who were tested for the virus later this month.
Patients who tested positive and negative will complete questionnaires asking about ongoing symptoms and returning to normal life. “We are looking for the characteristics of those who tested positive,” professor O’Donnell added. “However, we will not be able to tap into those not tested.”
Very few early Long Covid sufferers not admitted to hospital had a test, says Lesley Macniven, a founder of Long Covid Scotland, and they have no documentation to prove they had Covid and are now enduring long-lasting symptoms.
The writer and diversity consultant from Edinburgh said people struggling with chronic fatigue and other debilitating symptoms have been dismissed by doctors and researchers as they pleaded for help and support.
“The lack of availability of tests in the first wave has led many to be unable to prove they had the virus and are often unable to be diagnosed and treated with Long Covid.
“Patients are often having to hunt for supportive GPs to accept their account of having had Covid. In effect, we are being penalised for lack of testing provision that was the fault of the government. Now they have to shout to be recognised.
“A year later many have still not had an assessment or had their prolonged symptoms investigated. Those who had a positive test appear to have had an easier journey though they may still not find much in the way of treatment.”
The Royal College of GPs (RCGP) has called for better recognition of Long Covid. Dr Gail Allsopp leads on Long Covid for the RCGP and said it was wrong that patients were being denied treatment because they don’t have a positive test.
“I am saddened to hear these stories. It is important patients keep talking out loud,” she said. “The frustration is not just with patients but with clinicians on the ground. I myself, as a GP, have tried to refer patients to have these patients told they are suffering with anxiety.”
The struggle to get adequate treatment for Long Covid is verified by chronic fatigue charity, the ME Association.
Ewan Dale, from the charity said: “People with Long Covid are approaching us but there is no place to send them.
“Some are being advised by GPs to exercise when evidence shows that post-viral fatigue needs rest, not exertion, to recover.
“There seems to be little guidance on how to treat patients. Many were not desperately ill with Covid but now have chronic symptoms worse than the virus.
“Some have long-term organ damage and need ongoing medical care, not an eventual referral to an occupational therapist.”
Scottish Intercollegiate Guidelines Network (Sign), the National Institute for Health and Care Excellence, the English equivalent, and the RCGP have issued joint guidelines on the treatment of Long Covid.
Sign, which is part of Healthcare Improvement Scotland, said: “Evidence from patient experience has shown that many people feel their symptoms are not taken seriously by GPs when discussing Long Covid. The national guideline published in December 2020 recommends that clinicians take time to listen and show empathy.
“The guideline recognises that many people who had acute Covid-19 were not tested, particularly earlier in the pandemic. As a result, the guideline is clear that people should not be excluded from a Long Covid assessment, or for further investigations or specialist input, based on the absence of a positive Covid-19 test.”
The Scottish government says it supports developments of clinical guidance on long-term effects of Covid but wants patients to be treated near home by GPs, physiotherapists and occupational therapists and speech therapists.
“Unlike other major chronic illnesses, like rheumatology, cardiology and dermatology, care will not be centralised in teaching hospitals or specialist clinics.
“Our approach is for people to have access to the support they need for assessment, diagnosis, care and rehabilitation in a setting close to their home,” said a spokesperson.
A year on, I can’t leave the house but all doctors can do is tell me to take it easy
– Sufferer Barbara Melville
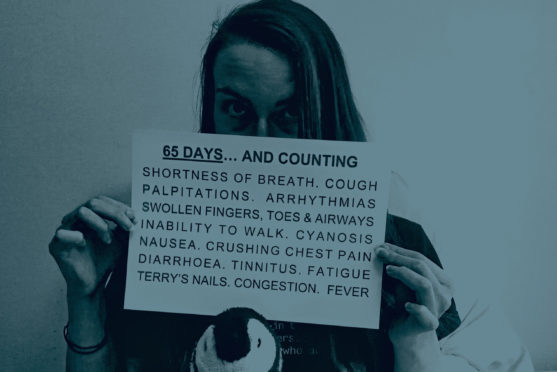
Barbara Melville discovered Long Covid had inflicted heart damage when she joined a Oxford University study to examine to examine the condition’s impact on organs.
She got the virus in April and mild symptoms like coughs, flushes and sniffles built into chest pain and breathing difficulties, so bad she could not walk and was bed-bound.
The science and literature lecturer and writer, who runs Long Covid Scotland, said: “My scan showed evidence of myocarditis – inflammation of the heart muscle.
“There were also a few abnormalities in my blood work but my other organs were in much better shape. I sent the results to a private cardiologist and my echocardiogram showed good heart function.
“The only advice was to take it easy and avoid exercise.”
A year on she is still only able to walk around her house when previously, she had trained in martial arts and hill-walked.
“Even walking or standing for a minute or two causes significant heart rate and breathlessness. I got no treatment but lifestyle advice. Others have had heart medication. I worry that those with heart issues aren’t being picked up, and it could be exacerbated by exercise. It’s important GPs, cardiologists and physiotherapists know about the emerging evidence.”
She is calling for an integrated service that diagnoses, treats, and supports recovery. She said: “Many support clinics, but whatever is developed needs to have co-ordinated, integrated services at the heart, informed by lived experience.”
The Oxford study – known as Coverscan and involving 200 patients – discovered damage to the pancreas, liver, heart and kidneys in Long Covid patients. Dr Rajarshi Banerjee, lead researcher, said: “It was done through quantitative MRI scans which allowed us to measure tissue characteristics and fibrosis in internal organs.
“It is vital to diagnose abnormalities, especially in patients who may be at risk of diseases like diabetes through a damaged pancreas.
“Untreated diabetes can damage eyes, kidneys and other organs. Pancreas damage may also account for chronic exhaustion.”
What happens where
No Scottish health board currently offers a dedicated Long Covid clinic. Instead, patients are treated in a variety of ways depending on where they live.
NHS Lanarkshire says it has a rehabilitation group to look at Long Covid and takes part in the National Rehabilitation strategy group set up by the Scottish government and university research into treating patients locally. It is also looking to help those with mental and physical illness due to lockdown.
NHS Greater Glasgow and Clyde says its InS:PIRE programme treats Covid survivors in a five-week plan for recovery after the Intensive Care Unit. Physical and psychological rehab is also offered to all.
Highland treats Long Covid with rehabilitation teams and has a small clinical team reviewing evidence nationally and locally. Borders has appointed a Covid lead clinician to work to deliver treatment. Outpatient and home services are being used through occupational, physiotherapy, speech, language therapists along with district nurses and GPs. Ayrshire and Arran says it treats patients through GP practices and other community health services.
Tayside has hospital care for patients after ICU and other emergency care and physiotherapist and occupational support in the community.
NHS Grampian said: “We are looking at the longer-term effects of Covid-19, and how we can best serve those patients.” NHS Western Isles is at the early stages of planning treatment, including physiotherapy, along with Shetland and Orkney health boards. It said that it will consult Long Covid charities in designing it.
NHS Lothian’s treatment includes hospital rehabilitation, psychological support and community rehab. NHS Forth Valley has a range of services, including rehabilitation teams, and NHS Dumfries and Galloway provides support through specialist teams, including virtual rehab classes and one-to-one appointments for specific issues, and developing self-management.
England has Long Covid clinics but there are none here
– Sufferer Maria Timony
Community nurse Maria Timony, 45, from Airdrie, has suffered from Long Covid since contracting the virus in June.
The hospice nurse and mum-of-four says she has experienced splitting headaches, fatigue and chest pain so bad she was admitted to hospital where a test suggested blood clots.
“It was found to be negative in scans but left the question of why tests proved positive and what else could have driven that result,” she said. “I got a negative Covid test in hospital but was later told that it may have been taken at the wrong time. I have never been referred to a Long Covid clinic – there are none in Scotland.
“England has these clinics and a lot of people here in Scotland are disappointed to see patients getting multi-disciplinary team care when we are not. That’s the care you what you need when you are unwell.
“GPs don’t have a lot of guidance on long Covid. I have a mixture of very good and not so helpful treatment and consultations are held online.”
Maria, returned to work on Thursday for the first time for four hours, looking at patient’s case notes from her home.
“My managers are very supportive but community nursing teams are extremely busy so I want to be back helping my colleagues.”
Another Long Covid sufferer, Lily Burns, from Fort William, says she has now been referred to Raigmore Hospital in Inverness for rehabilitation when local treatment failed.
The talented hairstylist was only 21 when she became desperately ill with Covid last April and was transferred to ICU in Raigmore. Her vital organs were being attacked by the virus, particularly her heart.
She said: “In the weeks after leaving hospital I felt I was recovering but fatigue and Long Covid has set in. Local treatment has not helped and I am now being referred back to Raigmore.
“This is obviously something that needs specialist care. My dad will drive me to the hospital for appointments.”
Researchers: More women are suffering
Women are five times more likely to suffer Long Covid than men, according to the latest research by Glasgow University.
Seven in 10 patients needing hospital treatment for Covid suffer symptoms up to five months later, with middle-aged women more likely to endure ongoing problems.
Dr Tom Drake, a research scientist and surgeon, said: “Research showed that women under 50 are five times more likely to experience ongoing fatigue and breathlessness.
“These were patients severe enough to be treated in hospital but not all were ill enough to be admitted to ICU. They were followed up for an average of 223 days and we found that acute fatigue and breathlessness were a lot higher than expected. Depression and anxiety were also evident.
“Around 82% reported fatigue. Not all of them had previous illnesses before going on to develop symptoms.
“We know that ongoing inflammation in the body can cause fatigue and breathlessness.
“Women have a more robust response to fighting off infection and it could be that this overdrive reaction is what is causing the symptoms of fatigue and breathlessness.
“More research is needed to find out if this is the case, another cause is responsible or the symptoms are driven by a combination of this and others factors.
“Research is also needed into whether a patient’s genetics makes them more susceptible to getting chronic post-Covid viral illness.
“Ongoing symptoms after surviving Covid is not driven by age or existing illnesses in patients, unlike survival from the virus.”

Enjoy the convenience of having The Sunday Post delivered as a digital ePaper straight to your smartphone, tablet or computer.
Subscribe for only £5.49 a month and enjoy all the benefits of the printed paper as a digital replica.
Subscribe © Stewart Atwood Photography
© Stewart Atwood Photography
