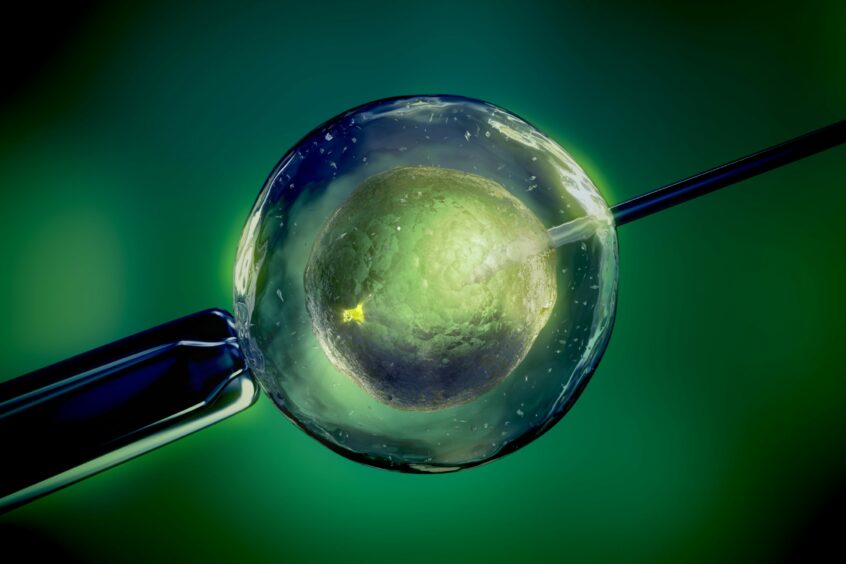
Women could be spared hormonal fertility treatments in future after scientists in Scotland grew human eggs in the lab.
Reproductive biologist Professor Evelyn Telfer and her team at Edinburgh University have spent more than a decade perfecting a method of stimulating ovarian tissue cells to produce eggs.
Now they are on the brink of testing the technique in sheep – and hope to be in a position to start human trials within five to 10 years.
“This is a technology of hope,” said Telfer, who was made a CBE for services to female reproductive biology last year. “Eventually, if it’s effective and safe, it could be used in a whole range of patients.”
It is hoped the development could eventually mean women undergoing fertility treatment in future avoiding the hormonal rollercoaster of artificial stimulation.
With the new technique, women would only need to undergo one small surgical procedure to remove a sample of ovarian tissue. This would contain “thousands” of immature eggs which could be stimulated in the lab so they are ready to be fertilised.
“With this procedure, once you’ve done it, you have it (the tissue sample),” said Telfer. “From a single biopsy you can do several cultures to obtain eggs so if it didn’t work on one occasion you could keep going back. Whereas with IVF, you may have to go through cycle upon cycle.”
Currently, IVF patients must have repeated hormone injections to stimulate egg production in the body and then undergo minor surgery under sedation so the eggs can be harvested. These are then fertilised with sperm in the lab.
But artificial hormones can cause side effects including low moods and headaches, as well as carrying the risk of hyperstimulation syndrome which can trigger dangerous blood clots or breathing difficulties.
The process typically only produces up to 15 eggs per cycle depending on the patient’s age. And if one cycle fails, patients have to go through the process again for every subsequent cycle.
While the new technology has the potential to revolutionise fertility treatment, it must be proven to be safe and effective before it can be used in humans.
Researchers are now ready to test whether lab-grown eggs can be fertilised and lead to viable pregnancies and the birth of healthy babies in animals. Previous studies have shown the technique works in mice.
But this year the Edinburgh team is joining with researchers at Leeds University to become the first in the world to trial the treatment in sheep, whose reproductive cycles are similar to humans. If it is shown lambs can be born and grow up without genetic defects, scientists will seek approval from fertility and medical regulators to begin human trials.
The research is primarily focused on finding a way of preserving the fertility of girls with childhood cancer ahead of chemotherapy or radiotherapy, which can render them infertile.
Female cancer patients in Edinburgh – some as young as 18 months – were the first in the world to receive the chance to freeze their ovarian tissue ahead of cancer treatment.
Telfer, recipient of the Distinguished Scientist award from the Society of Reproduction and Fertility in 2018, said she was hopeful girls storing their tissue today would be able to access the new treatment by the time they are old enough to have children.
“My hope is that this technology will be available within 20 years,” she added.
Sarah Norcross, director of the fertility research charity Progress Educational Trust, said growing human eggs in the lab was “extremely challenging” but that the research “showed promise” and offered hope to cancer patients.
She added: “The safety and efficacy of using lab-grown eggs will have to be rigorously tested before they can be used to try to achieve a pregnancy.
“If such tests are satisfied, and if lab-grown eggs are used successfully in treatment, then they might eventually be used more widely.”

Enjoy the convenience of having The Sunday Post delivered as a digital ePaper straight to your smartphone, tablet or computer.
Subscribe for only £5.49 a month and enjoy all the benefits of the printed paper as a digital replica.
Subscribe